ABSTRACT:
Fibrous dysplasia (FD) is a bone disorder in which fibrous connective tissue replaces normal bone. This is an anomaly caused by bone-forming mesenchyme characterized by a defect in osteoblastic differentiation and maturation. it is a non-neoplastic, developmental disease of the bone that begins in childhood with obscure aetiology. Clinically, it is presented as a continuously growing, painless mass at late childhood. Maxilla and mandible are mostly involved in the facial skeleton. Involvement of the zygomatic bone is rare. Fibrous dysplasia of the zygomatic bone may cause orbital dystopia, diplopia, proptosis, loss of visual
acuity, swelling, mass formation, or facial asymmetry. This report describes the case of a 34-year old male patient who had presented himself with painless swelling of left lateral frontozygomatic suture i.e. lateral buttress of midface and was diagnosed with FD with the help of CT scan of the face with 3D reconstruction and histopathology.
Key words: Nonhereditary, Frontozygomatic Suture, 3D Reconstruction, Mccune-Albright Syndrome, Cafe Au Lait Spots.
This article may be cited as:
Mukherjee S, Chatterjee J. Fibrous Dysplasia of a Craniofacial Complex: Case Report. J Adv Med Dent Scie Res 2020;8(7):92-94.
INTRODUCTION
Fibrous dysplasia is an uncommon nonhereditary, skeletal developmental anomaly in which normal bone is replaced by an excessive proliferation of cellular fibrous tissue intermixed with irregular bony trabeculae. It’s going to arise as one lesion called as monostotic or can occur with multiple lesions that affect
many bones which is often called polyostotic. A little set of polyostotic FD (fibrous dysplasia) also can occur as a multisystem developmental disorder called
McCune-Albright syndrome which is sometimes related to endocrine hyperfunction and cafe au lait spots.1 It seems to be a rare disease with an incidence of 1:4000–1:10,000 2 Craniofacial FD (CFD) affects the bones of the craniofacial complex, that included the mandible and maxilla, cranial base and vault, it’s one among the various styles of FD. 3 FD of bone occurs thanks to the missense mutations in Gs alpha gene in pluripotent embryonic stem cells. The inheritance of those mutations remains in a very population of postnatal skeletal stem cells or mesenchymal stem cells that help in directing the formation of atypical bone. 4 there’s a small female predilection for this condition.2 The bones which are commonly involved are maxilla and mandible, involvement of the ethmoid, sphenoid, frontal and temporal bones are infrequent. The affected bones show expansion, thickening and sclerosis. looking on the involved bone patients may suffer from visual abnormalities, hearing disturbances, facial asymmetry and tooth displacement.5 We report a case of
CFD in a very 34-year-old male patient.
CASE RERORT-
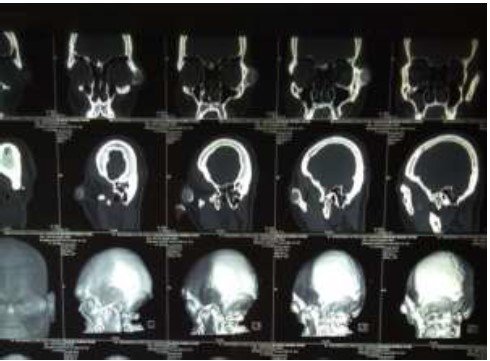
A 34-year-old male patient presented at the OPD with the complaint of painless swelling at the left border of the eye since the last 3 years. There was no history of trauma and paresthesia was noted down. Clinically pronounced facial asymmetry with a bony swelling in the left zygomatic bone involving left lateral frontozygomatic suture is noted. Diplopia or loss of visual acuity is not found. Proptosis was noted. (Figure 1) An excisional biopsy was obtained from the lesion in the zygomatic bone and histopathological analysis was done. Macroscopy showed two pieces of bony hard-tissue greyish white in colour. Larger measuring 1.5 cm × 0.8cm × 0.5 cm approximately. (Figure 2) 3D computed tomography shows a unilocular radiolucent expansive mass with radiopaque spicules, the characteristic focal area of ground glass appearance is noted involving the left zygomatic bone.


No involvement of any other bones in the skeleton noted. (Figure 3) Histopathological examination of the excised bone specimen showed curvilinear trabeculae of woven bone in a hypocellular fibroblastic stroma giving the characteristic Chinese letter pattern, confirming the diagnosis of fibrous dysplasia. No osteoblastic rimming noted. No evidence of atypia or raised mitotic count seen. (Figure 4) The current gold standard for the diagnosis of FD is a histologically-proven fibro-osseous lesion with poorly defined margins which are confirmed by radiographic findings.
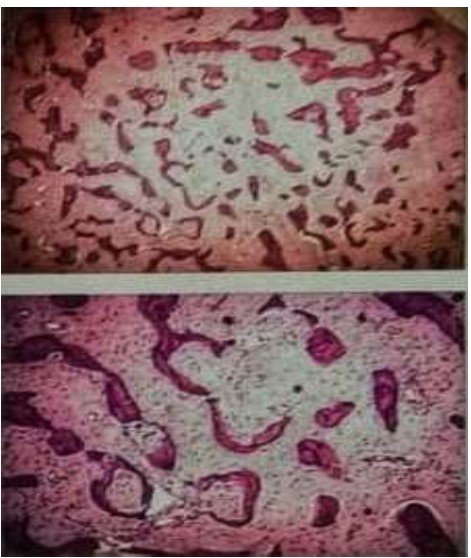
irregualar bony trabeculae
DISCUSSION
FD is a congenital, metabolic, nongenetic disturbance anomaly caused by bone-forming mesenchyme characterized by a defect in osteoblastic differentiation and maturation. 5 It represents 2.5% of all bone tumours and over 7% of all benign bone tumours. FD involves the facial and cranial bones in nearly 50% of PFD
patients and in 10%–27% of MFD patients.6 Maxilla and mandible are commonly affected with the temporal bone involved in 18% of cases. FD can occur at any
age. However, it is usually observed in children and young adults with 75% of patients presenting before the age of 30.6 No gender predilection is found. The typical radiographic feature of FD is a radiolucent, hazy or ground-glass, pattern. The patterns are due to defective mineralization of immature abnormal bone and it is usually different from the radiographic appearance of normal bone.5 The microscopic appearances are those of a hypercellular and cytologically uniform fibrous stroma within which delicate and irregularly shaped trabeculae of woven bone are deposited. The configurations of these bony trabeculae are often referred to as resembling Chinese characters.5,6 Treatment protocols for FD include observation, medical treatment, and surgery. Clinical observation is
suggested for FD lesions that have no risk of pathologic fracture or deformity. Medical treatment with bisphosphonates may have benefits including
improvement of function, pain relief, and lower fracture risk in appropriately selected FD patients. One study reported clinical improvement in children and adults treated with bisphosphonates.7 Surgery is indicated for confirmatory biopsy, correction of deformity, prevention of Pathologic fracture, and/or elimination of symptomatic lesions. Conservative management has been the standard of care, which involves removing the diseased bone via an intraoral approach. After a confirmatory biopsy of excised bony tissue, this case was diagnosed with symptomatic MFD. regular recall and clinical observation as been suggested. The reported prevalence of malignant transformation of FD is 0.4%–4%. Therefore, periodic follow-up, for example, every 6 months, and radiographic examination should be carried out to verify that there is no progression or malignancy.
REFERENCES-
- Waldron CA. Fibro-osseous lesions of the jaws. J Oral
- Maxillofac Surg. 1985 Apr;43(4):249-62
- Brannon RB, Fowler CB. Benign fibro-osseous lesions: a
- review of current concepts. Adv Anat Pathol. 2001
- May;8(3):126-43
- Speight P.M, Carlos R. Maxillofacial fibro-osseous
- lesions .Current Diagnostic Pathology 2006;12:1-10.
- Eversole R, Su L, ElMofty S. Benign fibro-osseous
- lesions of the craniofacial complex. A review. Head Neck
- Pathol. 2008 Sep;2(3):177-202
- PINDBORG JJ. Fibrous dysplasia or fibro-osteoma;
- report of a case. Acta radiol. 1951;36(3):196-204.
- doi:10.3109/00016925109176978
- Yang HY, Su BC, Hwang MJ, Lee YP. Fibrous dysplasia
- of the anterior mandible: A rare case report. Ci Ji Yi Xue
- Za Zhi. 2018;30(3):185–187.
- doi:10.4103/tcmj.tcmj_57_18
- Dua N, Singla N, Arora S, Garg S. Fibrous dysplasia of
- maxilla: Report of two cases. J Indian Acad Oral Med
- Radiol 2015;27:472-5.
- Chandavarkar V, Patil PM, Bhargava D, Mishra MN. A
- rare case report of craniofacial fibrous dysplasia. J Oral
- Maxillofac Pathol. 2018;22(3):406–409.
- doi:10.4103/jomfp.JOMFP_211_18






